Contents
- 1 SLAP Tear Simplified
One-stop resource: from Pain to performance
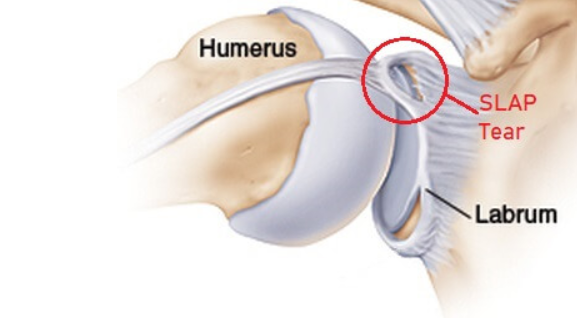
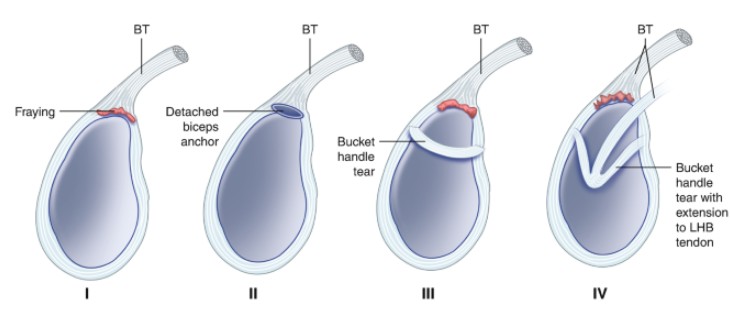
- 1.1 What exactly is a SLAP Tear?
- 1.2 How Do SLAP Tears Happen?
- 1.3 What are all the symptoms experienced by the patient?
- 1.4 Diagnosing SLAP Tears:
- 1.5 What is the best treatment approach?
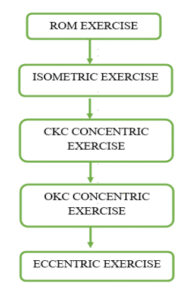
- 1.6 Rehabilitation
- 1.7 Reference
Azarudheen is a passionate physiotherapist and exercise prescriptor with a deeply rooted belief in the transformative power of movement and education. His journey began in 2013 as a first-year physiotherapy student, balancing academics with part-time work to support his ambitions. Early in his career, he sought practical experience and began working at a fitness center, eventually transitioning into roles that expanded his knowledge and skill set in both clinical practice and teaching.
Driven by a relentless curiosity and desire for growth, Azarudheen took on an anatomy tutor position, believing in the value of continuous learning. A pivotal turning point came with his experience in cardiopulmonary rehabilitation at PSG Hospitals, where he worked closely with lung transplant patients. This experience emphasized the life-changing impact of functional movement and patient education, inspiring him to dive deeper into respiratory and cardiovascular physiology.
With strong support and belief in his vision, Azarudheen pursued a Master’s in Exercise and Sports Science at Manipal University—choosing it over conventional MPT programs to focus more on biomechanics, exercise physiology, strength and conditioning, and lifestyle health. His dedication was evident as he spent late nights at the library, worked part-time in gyms and cricket academies, and honed his craft through practical application.
In 2022, despite initial doubts, he opened his first clinic in his hometown—an act of courage and self-belief supported by his family and mentors. Built from the ground up, this clinic marked the start of a new era. Today, Azarudheen leads a growing team of 21 physiotherapists across two thriving clinics in Chennai and Coimbatore. His philosophy centers on patient education, movement optimization, and professional growth, and he continues to evolve both as a clinician and a leader.
Azarudheen’s journey reflects the power of perseverance, vision, and lifelong learning. He is not only a practitioner but also a mentor and advocate for a more thoughtful, movement-centered approach to healthcare.