Every physio experiences moments of uncertainty, self-doubt, and low confidence, even with high grades, practical skills, knowledge, and more certificates. That’s because physiotherapy isn’t just about treatments, but it’s more about the therapist. Not all physios are the same, and it’s often the little things that make a big difference. So, what makes someone the best physio? This blog reveals that secret—and it’s exactly what we practice in our clinic, too. Let’s dive in.
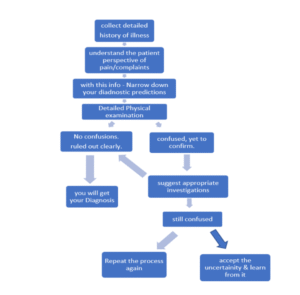
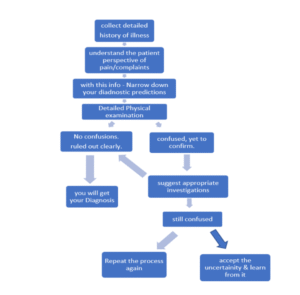
1) ASSESS, DON’T ASSUME:
The most common error in the medical field is MISDIAGNOSIS.
In reality, the first line of treatment begins with a proper diagnosis. Yet, many of us still fall into the habit of making assumptions based on stereotypical thinking about certain conditions we commonly encounter.
However, it’s crucial to look deeper beyond what is obvious. Because not every shoulder pain is a PA shoulder or a rotator cuff tear. Not every knee pain is osteoarthritis. And not every case of low back pain is due to a disc bulge.
There are a lot of things we tend to neglect during assessment. So, the best way to avoid misdiagnosis is to avoid predetermining a condition and jumping to conclusions. Instead, assess thoroughly and rule out all possible differential diagnoses with an open and critical approach.
“Not Every Knee Pain is Arthritis”
 2) TREAT THE PERSON, NOT JUST A PATIENT:
2) TREAT THE PERSON, NOT JUST A PATIENT:
If someone close to us, such as a family member, friend, or relative, is suffering, we naturally worry deeply and care deeply about their feelings. It should be the same with our patients, too, because a patient is also a person, not just a medical case.
Many healthcare professionals focus more on reports and investigations rather than truly listening to their patients. But one of the biggest disappointments for patients is not being heard.
As physiotherapists, we spend more time with patients, which makes us responsible for showing empathy, taking time to listen, and respecting their pain and emotions.
When we explain a condition, we have to adjust our communication based on the patient’s personality. Use simple, clear language instead of complicated medical terms, which can create confusion, fear, or anxiety.
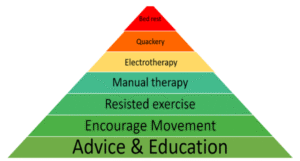
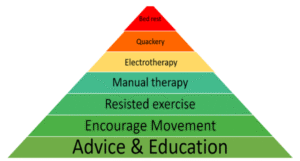
3) APPLY THE BIO-PSYCHO-SOCIAL MODEL(BPS)
Many physiotherapists strongly believe that pain is mainly due to tissue damage or biomechanical issues. But in reality, two people with the same issue or tissue damage often feel and express pain differently. Why? Because there’s something more than just the biomechanical issues that cause pain.
Humans are not machines. We can’t simply repair or replace a problematic part, and everything goes back to normal. Humans are influenced by thoughts, emotions, and life experiences. That’s why the psychosocial aspect is so important in treatment.
To help patients recover better, we must understand their mindset, emotions, and personal experiences. Educating patients and involving them in their care is key.
The same treatment won’t work for everyone. So, individualize the plan, address the psychosocial aspect, and prefer active approaches that empower the patient.
“There is no one-size-fits-all treatment
Because each individual is different .”
4) DON’T GIVE FALSE HOPE
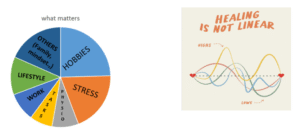
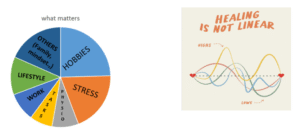
Everyone (both patients and physiotherapists) often wants a quick fix. But it’s important to remember that physiotherapy and healing are not like applying adhesive to fix a broken chair. The human body doesn’t always respond as we expect it to.
Sometimes, even a person with serious pathology can improve quickly, whereas a person with not-so-severe, non-specific pain may take longer than expected to see progress. This is because every condition/ tissue damage has a unique natural healing timeline, which also varies from person to person.
Also, the recovery and progression are influenced not only by what happens during treatment sessions alone, but also by what the individual does in daily life outside the rehabilitation center. So, the rehabilitation process is not always linear, and it is okay to have ups and downs in the progression.
Physiotherapists should consider these and be cautious not to give false hope or oversimplified solutions. Instead, we must help the patients set realistic expectations.
5) SELECT YOUR PATIENT WISELY
Not every physio needs to treat all kinds of patients (sports, musculoskeletal, neurological, paediatric-related, etc). Select your patients according to your interest, knowledge, skills, and experience. So that you can achieve better outcomes. Part of being a responsible physio is knowing when to say, “You may need someone else who’s a better fit for your needs.” So learn to say NO to your patients.
If you are running a clinic or hospital, select an appropriate therapist for each patient based on the factors mentioned above. It is recommended not to change the therapist frequently, as this will help the therapist to understand the patient completely and also build a strong therapist–patient relationship.
It is important to understand that we don’t have to treat all types of patients. Be it a sports injury, musculoskeletal conditions, neurological rehabilitation, cardiorespiratory physiotherapy, or pediatric care, one is expected to excel in all these. Based on your interest, knowledge, and experience, find your niche specialization, learn it, master it, and choose your patients accordingly. This yields better outcomes.
Part of being a responsible physiotherapist is knowing someone who’s not your patient and learning to say, ‘You may need someone who’s a better fit for your needs.’ Learning to say NO is a professional and respectful quality, enabling people to receive appropriate treatment and avoid excessive health care expenses.
If you manage a clinic or hospital, assign each patient to the most appropriate therapist based on suitability and not just based on availability. Also, frequently switching therapists mid-treatment should be avoided, unless necessary. It helps the therapist better understand the patient and helps build a good therapist–patient relationship, which is the basis of successful rehabilitation.

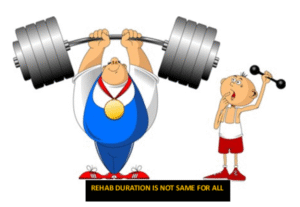
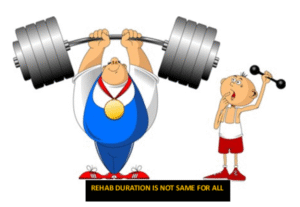
6) HOW OFTEN SHOULD THE PATIENT DO REHAB?
The number and frequency of the sessions are equally important as your treatment techniques. These cannot be standardized, because some chronic conditions, such as frozen shoulder and ankylosing spondylitis, take more time to heal. In such conditions, scheduling sessions daily is unnecessary and sometimes unwanted, in terms of therapeutic and financial aspects. Such patients need more education on self-management strategies, home programs, and lifestyle modifications. So, less number of sessions are sufficient.
However, in case the patient has a high fear of movement, anxiety, or struggles with psycho-social challenges, increasing the session frequency will be beneficial in building confidence and bringing out better outcomes.
While planning and scheduling the sessions, it is important to consider a lot of factors from the patient’s perspective, including the diagnosis, knowledge and understanding of treatment, personality, fear of movement, financial situation, fear of movement, and psycho-social concerns.
7) MONEY IS NOT A BIG DEAL
Of course, in today’s world, money drives everything, and people are constantly chasing it. But as physiotherapists, we shouldn’t play business card games with patients.
Our services should not be money-driven. When a patient can’t afford the cost of the rehabilitation, we can help them by planning the sessions accordingly. We can either,
- Reduce the cost or number of sessions
- Slowly taper or stop the sessions upon good improvement in the patient.
The Quality of the treatment speaks volumes, especially the empathy you show is more valuable than the specialized and fancy treatment techniques..

8) DON’T LIMIT YOUR TREATMENT GOAL:
Usually, our treatment will be driven by the patient’s needs and goals. But what if their goals are limited, like just wanting to reduce pain, or wanting to move their body a bit more? Our treatment should not be limited to that. The pain, if persistent, will make the person forget what they are capable of. The pain will trick the patient’s mind into believing that just pain relief is enough.
So, it becomes the physiotherapist’s responsibility to educate, give confidence, and show the patients that they can have bigger goals and are achievable.
Why just walk if you can run?
Whatever the condition the patient has, we have to help them take one more step higher. Along with their goals, you have to improve their physical activity, overall health, and wellbeing. Because true rehabilitation isn’t just about fixing problem, it’s about helping people live better, healthier, and more capable lives.
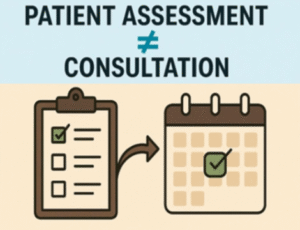
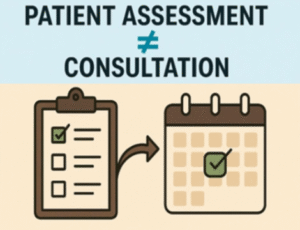
9) WHEN DO YOU HAVE TO ASSESS A PATIENT?
Mostly we think that only the first visit of the patient (consultation), is more about assessment. Then we get into the treatment part and never look back at the assessment part. Even when the patient does not improve, we’ll try to modify the treatment part alone.
We generally overlook the assessment, which is not just about identifying what’s wrong with the person’s body. Instead, it’s more about understanding the person in front of you as a whole. It is not possible to understand a human in just one meeting, that is why we should understand that every session is an assessment. Try to understand the person’s biomechanical and psycho-social aspect better in every session, to avoid misdiagnosis and to achieve best possible outcomes.
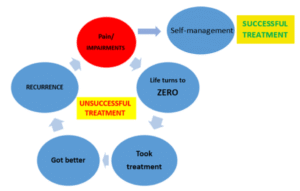
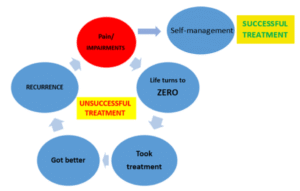
10) WHAT IS SUCCESSFUL TREATMENT?
Almost all therapists will reduce pain and improve functional ability, but can you assure the patient that they will not get the same pain/ injury in the future? No right! Because pain is multifactorial, we can’t completely prevent/predict the recurrence. Also, if the pain recurs, their life should not go back to zero.
Then, how to make the treatment successful? We can’t absolutely prevent the recurrence of an injury or pain. But we can ensure that when the person gets the same pain next time, he should be able to manage it himself (self-management), rather than rushing back to us. This reduces the patient’s dependency on physiotherapists and improves the person’s confidence and mindset. This is the true testimony of your successful treatment.
CONCLUSION
Being a great physio isn’t about having magical hands or fancy machines—it’s about being deeply human. The real secret? See the person as a whole, not just their pain/symptoms. Diagnose with depth, listen with intent, and treat with empathy. True success isn’t in how fast pain fades—it’s in how confidently a person moves forward after. Great physios create lasting change—not just in bodies, but in mindset, movement, and the way people live their lives.