ACL Non-Surgical Rehab
PATIENT PROFILE
Age:42
Gender: Female
Occupation: Housewife
Chief complaints: Complaints of instability in the left knee while walking fast and climbing stairs.
HISTORY
In March 2025, the patient fell from a bike and had severe injury to the left knee, resulting in pain and swelling over the joint. So, she consulted an orthopaedic doctor and underwent X-ray and MRI imaging. The X-ray was normal, but the MRI report suggested a Grade 3 ACL sprain. The doctor recommended rest and the use of a knee brace for a few days and advised surgery if the instability worsened. The pain and swelling decreased after a few weeks of rest, but the instability remains unchanged and affects her daily activities. She doesn’t want to have surgery.
Objective:
She wants to go back to normal day-to-day activities without surgery.
Physical Activity Status:
She goes for a walk, but not regularly. No other physical activity except that.
Sleep Level:
7-8 hours a day
Stress Level:
She is experiencing stress due to difficulty performing her daily activities and a lack of confidence in carrying out daily activities because of instability in her knee.
PAIN ANALYSIS
- Intensity: 3/10 (Pain < instability)
- Aggravating factors: Fast walking, stair climbing, getting on the bike.
- Relieving factor: Rest
- Location: Anterior part of the left knee
- Type of pain: Mechanical
- Irritability: High
- Sensitivity: Low
- Lifestyle impact: High, it affects her day-to-day activities.
- Fear of movement: Present. Fear of knee instability while performing deep squats, walking fast, and while getting on a bike.
TAKEAWAY FROM HISTORY AND PAIN ANALYSIS
The patient reports only mild pain; however, a heightened fear of instability is significantly impacting her daily activities, leading to psychological distress and reduced confidence.
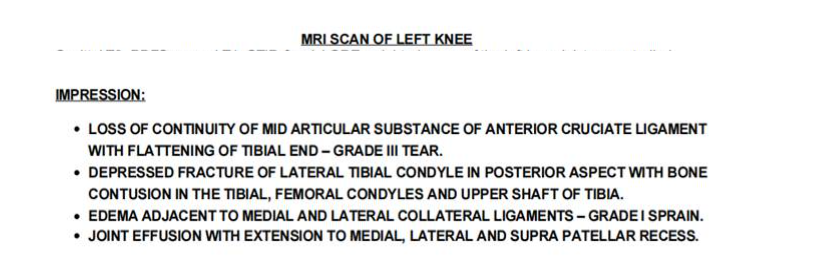
Although the MRI shows a grade III ACL sprain, the severity of the injury must be clinically correlated.
PHYSICAL EXAMINATION:
Observational findings:
- There is no swelling or redness present.
- Terminal knee extension and flexion have been reduced on the affected side.
Mobility screening:
- Forward bending – Good.
- Overhead squat – Bad. Unable to go deeper while squatting. Complete shift towards the right side
Strength test:
| Test | Right | Left | LSI |
|---|---|---|---|
| S/L squat | 8 reps | Unable to do | – |
| S/L hamstring bridge | 15 reps | 12 reps | 80% |
| S/L Glute bridge hold | 40 sec | 31 sec | 77% |
| S/L Calf raises | 16 reps | 12 reps | 75% |
| Side plank leg lift | 35 sec | 26 sec | 73% |
Special test:
- Anterior drawer test- Positive
- Lachman test-Positive
- Lever sign-Negative
INVESTIGATION:
DIAGNOSIS:
Belief and expectation of the patient:
The patient wishes to return to normal daily activities without undergoing surgery. She believes that exercise can aid in her recovery and expresses a strong desire to remain active.
Patient’s perception of pain:
She doesn’t have much pain; her major complaint was instability.
Psycho-social factor analysis:
- Cognitive: Affected, MRI shows a grade III ACL sprain, and she’s scared to go for surgery.
- Affective: Affected, the feeling of instability is affecting her daily life and making her stressed.
- Social: Not affected.
Diagnosis With Clear Explanation:
Anterior cruciate ligament injury -Grade 3
Explanation: The patient was presented with significant knee instability during daily activities, and Initial symptoms included pain, swelling, and difficulty with weight-bearing. Even though the pain and swelling got reduced eventually, she continues to experience a persistent sense of instability without the use of a knee brace. Functional limitations are noted in activities such as squatting, twisting, and sudden directional changes. MRI findings also confirmed a Grade 3 ACL tear.
TREATMENT PLANNING:
ACL surgical /non-surgical management decision-making
| Criteria | Interpretation | Scoring |
|---|---|---|
| Pain | During functional activity | 1 |
| Swelling | Not present | 0 |
| Knee flexion ROM | Passive is good | 1 |
| Terminal knee extension | Both active and passive are affected | 2 |
| Muscle mass | Not affected | 0 |
| Muscle strength | Unable to do a single-leg squat | 0 |
| Stability and balance | 50% stability compared to the unaffected leg | 1 |
| Instability episodes | >1 | 2 |
| Special tests |
● Anterior drawer test- Positive ● Lachman test-Positive |
2 |
| MRI findings | Grade 3 tear | 2 |
| Return to sports | Not needed | 0 |
| Opinion about surgery | Not interested | 0 |
| Total score: | 11 / 24 |
Percentage of scoring requiring surgery= 11/24 x 100 = 45.833%
- <50% – Start rehab. After three months of rehabilitation, if necessary, go for surgery.
- >50% go for surgery – consider rehabilitation before surgery
So, the decision has been made to start ACL non-surgical rehabilitation.
- How long it will take to cure (research /evidence-based): 3-5 months
- How many sessions: 35-40 sessions, 12-week plan
Things to be focused on during treatment:
Patient education about recovery helps overcome fear and promote confidence in her daily activities, as psychological readiness plays a major role in recovery.
Training the uninjured limb is also important
Don’t keep any time-based criteria and always go with individualisation principles
Treatment strategy:
| Week | Sample Exercise Program |
|---|---|
|
1-3 weeks Primary focus: Knee ROM exercises and isolated muscle strengthening |
● Supine quad sets ● Standing knee extension with a ball ● Prone lying quad extension ● Seated leg extension with loop band ● Wall squat ● TKE with band ● SLR ● Heel slides ● Banded prone knee flexion ● Cycling |
|
4-8 weeks Primary focus: Progressive lower limb strengthening exercises |
Quadriceps: ● Retro walk ● Wall squat ● Deep squat ● S/L squat with support Hamstring: ● Prone banded Hamstring curl ● Hamstring curl eccentric ● Hams bridging ● RDL Hip extensor: ● Bridging, ● Fire hydrant Hip flexors: ● Long sitting SLR ● Banded marching Hip abductor: ● Clamshell ● Banded sidewalk Hip adductor: ● Side-lying leg lift ● Adductor ball press ● Sumo squat Ankle plantar flexion: ● Standing calf raises ● Seated calf raises Ankle dorsiflexion: ● Shin raises ● Banded dorsiflexion |
|
9-12 weeks Primary focus: Focus more on unilateral strengthening and starting jogging/running |
● S/L squat ● Bulgarian split squat ● Lunges (forward, reverse, lateral) ● Walking lunges ● Nordic/Reverse Nordic ● Dead lift ● Single-leg RDL ● Side plank leg lift hold ● Copenhagen plank ● Single-leg calf raises ● Loaded DF |
Return to run test:
3 months after rehab:
Benchmark to start running:
- Limb Symmetry Index is >80% in all tested muscles of LL.
- Single leg hopping: >10
Strength test:
| Test | Right | Left | LSI |
|---|---|---|---|
| S/L squat | 20 | 19 | 95% |
| S/L hamstring bridge | 35 | 35 | 100% |
| S/L Glute bridge hold | 57 sec | 54 sec | 94% |
| S/L Calf raises | 28 | 26 | 92% |
| Side plank leg lift | 55 sec | 54 sec | 98% |
Single leg hopping:
< 5 (Patient had a lack of confidence to jump on a single leg)
Findings after RTR test: Even after achieving limb symmetry of more than 80% compared to the unaffected side, the patient still lacks confidence in single-leg hops, which indicates the patient needs more plyometrics and single-leg stability-focused exercises in the upcoming sessions for a better outcome.
Upcoming plan
13-17 weeks :
- Focus more on single-leg exercises and plyometrics, along with patient education, to build more confidence.
- Continue progressive strength training for LL weekly, 3 days, including 1-day plyometrics-focused exercises.
- Weekly 2-day Cardio exercise -Jogging, Running, rowing, cycling, etc