Case Of Torn-loose Shoulder
PATIENT PROFILE:
Age and gender: 31years / male
Occupation: social worker (predominantly desk-based job)
Complaint: Left shoulder pain
HISTORY:
The patient presented with long-term pain in the left shoulder, associated with a history of recurrent shoulder dislocations.
In 2012, while playing handball, the patient sustained a traumatic anterior shoulder dislocation following a collision with three players. The shoulder was relocated on-field by the coach, and the patient was advised to wear a sling. However, no structured rehabilitation was undertaken. Following this incident, the patient avoided weightlifting and activities involving overhead movements.
After six years, in 2018, the patient experienced a recurrence of shoulder dislocation while lifting a heavy rice bag. He sought physiotherapy care, where the shoulder was relocated, and modalities such as IFT and ultrasound were administered for seven days, with minimal pain relief.
Subsequently, a physiotherapist friend assessed him and suggested a diagnosis of periarthritis of the shoulder. Exercise-based treatment was initiated, but symptoms worsened, and he became unable to perform basic activities such as riding a bike.
The patient later consulted an orthopaedic surgeon and underwent a PRP injection in April 2023. Although he regained the ability to ride a bike, pain persisted. He was prescribed steroids for approximately 1.5 years, yet his symptoms failed to resolve.
The patient reports progressive fear, apprehension, and functional avoidance of the left shoulder.
Relevant Background Information
- Past Medical/Surgical History: He has a history of recurrent shoulder dislocation
- Physical Activity Level: Sedentary
- Sleep: 5–6 hours; disturbed sleep due to pain when lying on the affected side
- Stress Levels: High, related to persistent pain
- Previous Treatments: Multiple consultations, physiotherapy modalities (IFT, US), PRP injection, long-term steroid use
- Patient’s Goal: To be pain-free and regain normal shoulder function
PAIN ANALYSIS:
- Intensity – 7/10
- Aggravating factor – Lifting heavy objects (water cans, rice bags), Overhead movements (>90° flexion, abduction, external rotation), Driving with jerky movements
- Relieving factor – rest
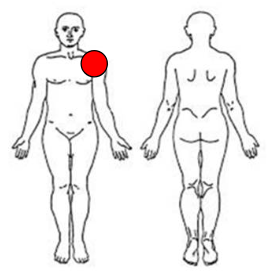
- Location: Diffuse pain in the Left Shoulder
- Duration – Chronic, the problem has been persistent for 13 years, but it has been severe for the past 2 years.
- Type of pain – nociceptive pain
- Character – intermittent pain, mechanical
- Irritability – low (pain started gradually after lifting above 90 degrees in flexion, abduction, and external rotation)
- Sensitivity – low (if he stopped doing overhead movement, then pain would subside)
- Lifestyle impact: Moderate level of impact. He can’t use his left shoulder during any functional activity.
- Fear of movement analysis – fear induced during external rotation, abduction, flexion above 90 and also lifting heavy weights.
Our understanding from the history and pain analysis:
The patient likely developed chronic shoulder instability following the initial traumatic dislocation due to a lack of rehabilitation, leading to recurrent dislocations, weakness, fear avoidance, and functional decline.
PHYSICAL EXAMINATION:
Observational findings:
Slight muscle atrophy on the left deltoid (reduced muscle bulk). No other visible changes like swelling, redness, or bruising.
ROM analysis:
AROM – restricted, painful in all directions on the left shoulder
| Right | Left | |
|---|---|---|
| Shoulder flexion | 180 degree | >170 degree (Painful) |
| Shoulder abduction | 180 degree | >170 degree (Painful) |
| External rotation | 100 degree | >80 degree (Painful) |
| Internal rotation | 90 degree | 90 degree |
Mobility screening
- Shoulder overhead flexion mobility: left side reduced
- Thoracic rotation: slightly reduced on the left side.
Stability screening
| Strength Test | RIGHT | LEFT | LSI% |
|---|---|---|---|
| Side lying Shoulder External Rotation (ER) – 1kg | 20 | 7 (Painful) | 35% |
| Shoulder press – 3kg | 17 | 4 (Painful) | 24% |
| Bench press – 3kg | 20 | 6 (Painful) | 30% |
| Lateral raise – 2kg | 19 | 7 (Painful) | 36% |
| Biceps curl – 3kg | 20 | 7 | 35% |
Palpation – No pain on palpation
Special tests
- The break test was positive on the left shoulder compared to the right shoulder [shoulder flexion, shoulder abduction, shoulder external rotation]
- SPRULING TEST – Negative
- UPPER LIMB TENSION TEST – Negative
INVESTIGATION:
MRI – Cervical Disc Bulge
DIFFERENTIAL DIAGNOSIS:
Stiff Shoulder - Ruled Out
- Mostly occurring in old age, above 45 years
- More common in women.
- Pain stimulates the affected side while the patient sleeps on the unaffected side.
- A stiff-shoulder patient will be unable to lift the full range actively
- The patient’s affected side may have a reduction of at least 30 degrees in elevation and 50 degrees in external rotation.
- Both AROM and PROM will be restricted in stiff shoulders.
Cervical radiculopathy - Rule out
- No radiating pain in the left side
- No numbness
- Spurling test negative
- ULTT was negative
DIAGNOSIS:
1) What is the patient’s perception of pain? He had a poor understanding, and he had apprehension.
2) Psycho-social factor analysis
| Cognitive | Highly affected (poor pain understanding) |
| Affective | Moderate affected |
| Social | Minimal Impact |
3) Belief and expectation from the patient
- Patient Belief: he attributes pain primarily to cervical disc bulge
- Expectation: Pain-free movement and functional recovery
4) Diagnosis With Clear Explanation
Unstable Shoulder (Torn–Loose Shoulder)
The patient has recurrent shoulder dislocations and multidirectional instability, resulting in pain, weakness, fear of re-dislocation, and significant functional limitation—especially during overhead activities. Long-term avoidance and sedentary behaviour have contributed to muscle weakness, apprehension, and poor motor control, leading to a painful and unstable shoulder.
Key Clinical Features Supporting Diagnosis:
- History of recurrent shoulder dislocations
- Painful and restricted AROM in all directions
- Significant strength deficit (LSI <40%)
- Positive break test
- High fear avoidance and poor pain understanding
TREATMENT PLANNING:
1) How long will it take to cure? Approximately 3 months.
2) How many sessions – 12weeks – 3 sessions per week
3) Things need to be focused on Treatment:
- Mobility restoration
- Shoulder and scapular stability
- Progressive strengthening (isometric → isotonic → eccentric → dynamic stability)
- Fear reduction and confidence building
4) Treatment planning strategy
| TIME FRAME | TARGET | SAMPLE EXERCISES |
|---|---|---|
| First week | Mobility with isometric exercises | Thoracic rotation mobility, thoracic extension, isometric exercises for external rotation and internal rotation. |
| 2nd week and 3rd week | Isometric progression, isotonic exercises with manual and scapular mobility. | Mobility exercises progression, side-lying external rotation activation with manual, lateral raise, shoulder press, prone V, T, W, and scapular push-up. |
| 4th week and 5th week | Progressive developing load and core muscle activation. | Banded external rotation, banded lateral raise, half-kneeling shoulder press, and banded rotation. |
| 6th week and 7th week | Start eccentric exercises | Crook-lying external rotation activation with the assisted opposite hand. |
| 8th week to 9th week | Start stability exercises | Shoulder tap, push-up, downward dog, toe touch. |
| 10th week to 12th week | Stability exercises progression with kettlebell | Windmill exercises, Turkish get-up, lunge kettlebell, press kettlebell, and single-leg standing kettlebell. |