LIPEDEMA IS NOT A RARE DIAGNOSIS, BUT MOSTLY A MISSED DIAGNOSIS
COMPLAINTS:
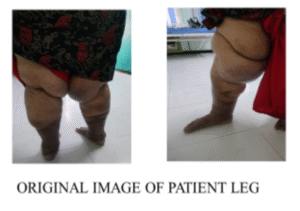
A 54-year-old female complained of excessive fat deposition in the proximal part of both legs and feeling heaviness in the legs while walking. She was unable to lie supine for 1 year. She came to reduce it with exercise after a doctor’s advice.
HISTORY:
She was diagnosed with pulmonary hypertension and obstructive sleep apnea 3 years ago. She has had varicose veins for 8 years and is undergoing treatment for the prevention of DVT. She has no history of surgery.
After her second delivery, in 1997, she became overweight. Currently, 8 months back, she started developing creases on the right thigh, which gradually increased in size. She already had a history of varicose veins, and she was diagnosed with venolymphatic edema in both legs.
When she went to another hospital, they suggested undergoing liposuction surgery to debulk the limb. As she had a pulmonary problem, she was not fit for surgery. Also, she was unwilling to undergo surgery. She is so obese, weighing 115 kg, and even walking increases friction between both legs. So, she came to us for conservative management.
She is very confused about her health as she has consulted many doctors, and she hasn’t received a clear explanation.
Previous physical activity status:
She is minimally active, doing some random exercise and walking around her apartment, only two rounds, covering nearly 1km. She couldn’t walk for more than 10-20 minutes due to breathlessness (a known case of pulmonary hypertension) and leg pain.
Sleep:
Sleep is affected as she has obstructive sleep apnea, so she has avoided sleeping in bed for the past 1 year.
Stress level:
- She was highly stressed, thinking that her condition might worsen during the summer season as the friction between her legs increased.
- She is confused whether it is curable or not; she fears the risk of infections and further development of the same in her left leg.
- She is not willing to have surgery. She has a financial burden and lacks family support.
The objective of consulting us was to reduce and manage the limb size and be able to lie down and sleep.
PAIN ANALYSIS:
- Intensity: 4/10
- Aggravating Factors: moving the limb after a long rest
- Relieving Factors: pain settles over time, no particular relieving factor
- Location: entire lower limb (bilateral- more on the right side)
- Duration: 8 months
- Type of Pain: nagging
- Irritability: low
- Sensitivity: low
- Lifestyle Impact: highly impacted as most of her ADLs are affected, but not so much because of pain.
Understanding the Patient’s Problem Based on History and Pain Analysis:
Having a lot of medical conditions will be psychologically disturbing. She has a lot of confusion and concerns about her health as she didn’t get a proper explanation of her condition.
We suspect that she has lymphedema, considering her limb size, its association with obesity, and varicose veins. However, further assessment will be conducted to rule out other potential diagnoses.
PHYSICAL EXAMINATION:
OBSERVATION:
- Shape of the limb: The proximal part of both limbs was huge compared to the distal part (distorted appearance, the right was more so)
- Infection: no signs of infection
- Spider veins: present on both legs, in the popliteal region.
- Discolouration: present in the distal part of both lower limbs.
- Skin folds and creases: present in the proximal part of the limb.
PALPATION:
- Type of swelling/oedema: minimal pitting in the distal leg
- Tenderness: present in the distal leg region
- Subcutaneous tissue changes: rubbery/fatty
- Skin condition: tissue thickened like fibrosis (no bump and no ulceration) in the distal leg.
ANTHROPOMETRIC MEASUREMENTS:
Waist circumference: 104 cm
Hip circumference: 145.5 cm
Waist-hip ratio: 0.71 (moderate risk for lipedema; Low risk for CVD)
However, the risk calculation based on the waist-hip ratio is not reliable as the person has increased fat around both her hip and waist (which is interpreted as a lower waist-hip ratio).
But considering her weight and BMI, it is evident that she is at higher risk for lipedema and cardiovascular diseases.
Also, lymphedema is characterised by distal swelling of extremities. But she has more proximal enlargement than distal, skin is more of a rubbery texture, not leathery, directing us away from lymphedema.
BMI: 44.9kg/m2
LIMB CIRCUMFERENCE: (tape measurement in cm)
| AREA | RIGHT | LEFT |
|---|---|---|
| CALF | 52 cm | 51.5 cm |
| POPLITEAL FOSSA | 68.5 cm | 56.5 cm |
| MID THIGH | 86 cm | 72 cm |
| GLUTEAL CREASE | 88.5 cm | 77.5 cm |
Special tests:
Stemmer’s Sign:
Negative (a fold of skin pinched and lifted at the base of the 2nd toe and the middle toe). Stemmer’s sign has 92% sensitivity; hence, a negative test helped in ruling out lymphedema.
In lymphedema, there is more fluid accumulation, so we couldn’t pinch the skin; here it is negative and making sure of not lymphedema.
FUNCTIONAL ASSESSMENT:
- Sit to stand: able to do without the support
- Walking: able to walk but not for a longer duration and distance due to breathing difficulty (less than 1km)
- Quality of walking: Moderately affected with reduced speed and reduced cadence
- Gait: waddling gait
- Ability to extend legs in high sitting: able to lift
- Use of aids: no
PSYCHOSOCIAL ASSESSMENT:
Cognitive: moderately affected
Affective: highly affected
Social: highly affected
INVESTIGATION:
Blood test:
| Test | Result | Normal range | Inference |
|---|---|---|---|
| ESR | 55 mm | <12 mm | Elevated |
| CRP | 11.6 mg/L | <5 mg/L | Elevated |
| Cholesterol | 257 mg/dL | <200 mg/dL | Elevated |
| Triglycerides | 182 mg/dL | <161 mg/dL | Elevated |
| LDL Cholesterol | 125 mg/dL | <100 mg/dL | Normal |
| HDL Cholesterol | 29 mg/dL | 42–88 mg/dL | Normal |
USG-DOPPLER:
There are a few dilated varicosities in both the sapheno-popliteal junction and the great saphenous vein.
DIFFERENTIAL DIAGNOSIS
Ruling out each potential diagnosis based on the differentiating features:
Lymphedema:
- It can be ruled out as it is often Unilateral, but she has bilateral involvement.
- The distal part is more swollen than the proximal,
- Stemmer’s sign is negative,
- Skin infection is common,
- Skin creases will be exaggerated, and
- Squaring of toes will be present.

Obesity:
- The entire body area of fat distribution will be present.
- No pain
- Responds to diet and exercise.

Congestive heart failure:
Bilateral leg swelling, but no distortion in the limb’s shape.

Cellulitis:
- Redness and temperature difference in swollen legs,
- Acute development

DIAGNOSIS:
Lipedema – associated with venous insufficiency
According to history and physical examination, the diagnostic features are related to lipedema overlapped with venous insufficiency.
Diagnostic features,
- It was a gradual onset and bilateral involvement
- The swelling stops at the ankle and wrist
- Subcutaneous fat deposition
- The presence of spider veins and a fold of fat
- Increased BMI and waist-hip ratio
- Discolouration and edema of the distal leg
- Fibrosis-like tissue thickening
Correlating with pathogenesis:
- According to the pathogenesis of lipedema due to adipocyte hypertrophy, there will be constriction of the capillaries.
- It will increase the peripheral resistance in capillaries, and it leads to increased blood vascular leak and increased lymph formation, so adipocyte hypertrophy leads to venous insufficiency.
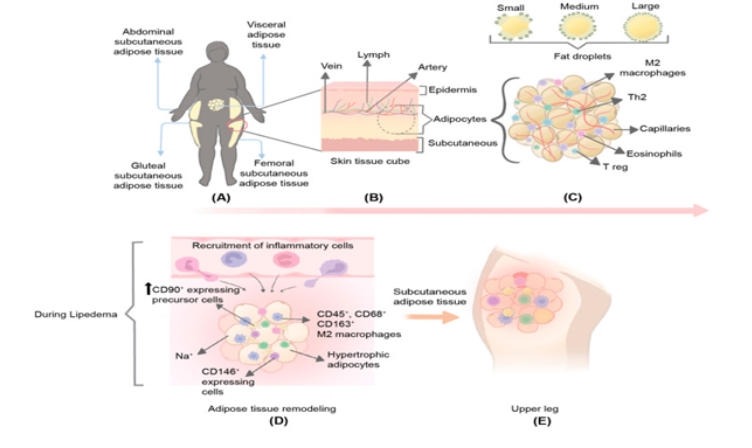
(Al-Ghadban, Sara et al. “Dilated Blood and Lymphatic Microvessels, Angiogenesis, Increased Macrophages, and Adipocyte Hypertrophy in Lipedema Thigh Skin and Fat Tissue.” Journal of obesity Vol. 2019 8747461. 3 Mar. 2019, doi:10.1155/2019/8747461)
Confirmation of diagnosis:
The diagnosis was confirmed as lipedema as the lipid profiles and inflammatory markers were high in the blood test
Suggested investigations for further confirmation:
MRI scan: It has to show subcutaneous fat with no fluid
Lymphoscintigraphy: To rule out lymphedema, normal lymphatic functioning is present in lipedema patients.
Biopsy of tissue: Adipogenesis may also contribute to mass increases, based on direct visualisation of increased adipose progenitor markers and cell cycle regulators such as CD34, ZNF423, ZIC1, UGT1A7, GREM1, TRIM67, and Bub1 in biopsied tissue.
Lipedema: A Current Understanding of Its Pathology and Natural History

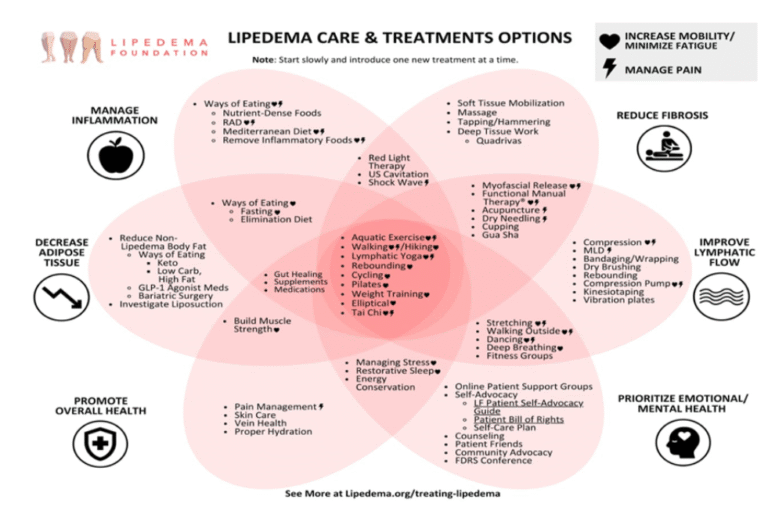
TREATMENT PLANNING:
It is a progressive subcutaneous adipose tissue disorder; it cannot be cured but only managed. So, we need long-term management to provide proper rehabilitation and improve the patient’s quality of life with a holistic approach.
For further evaluation and medical management, we have referred her to the filariasis management, ICMR-Vector Control Research Centre.
Potential Physiotherapy Treatment Strategy:
Self-management strategy:
- Maintaining limb hygiene, like a skincare routine, to avoid infection in the folded skin
- Improving functional activities
- Facilitating independence in Activities of daily living
Muscle strengthening exercises:
- Lower body strengthening is more important to improve the efficiency of venous pumping and avoid further complications like gangrene, venous ulcerations, etc.
- Improving lymphatic flow
- Reducing and managing inflammation
Breathing exercises and proper pacing between exercises:
Breathing exercises improve relaxation and the ability to recover between sets of exercises.
Others
- Prioritising mental health by giving optimistic care and support.
- Patient education: Explaining the nature of the disease and possible outcomes
- Garments and pneumatic compression
- Manual lymphatic drainage